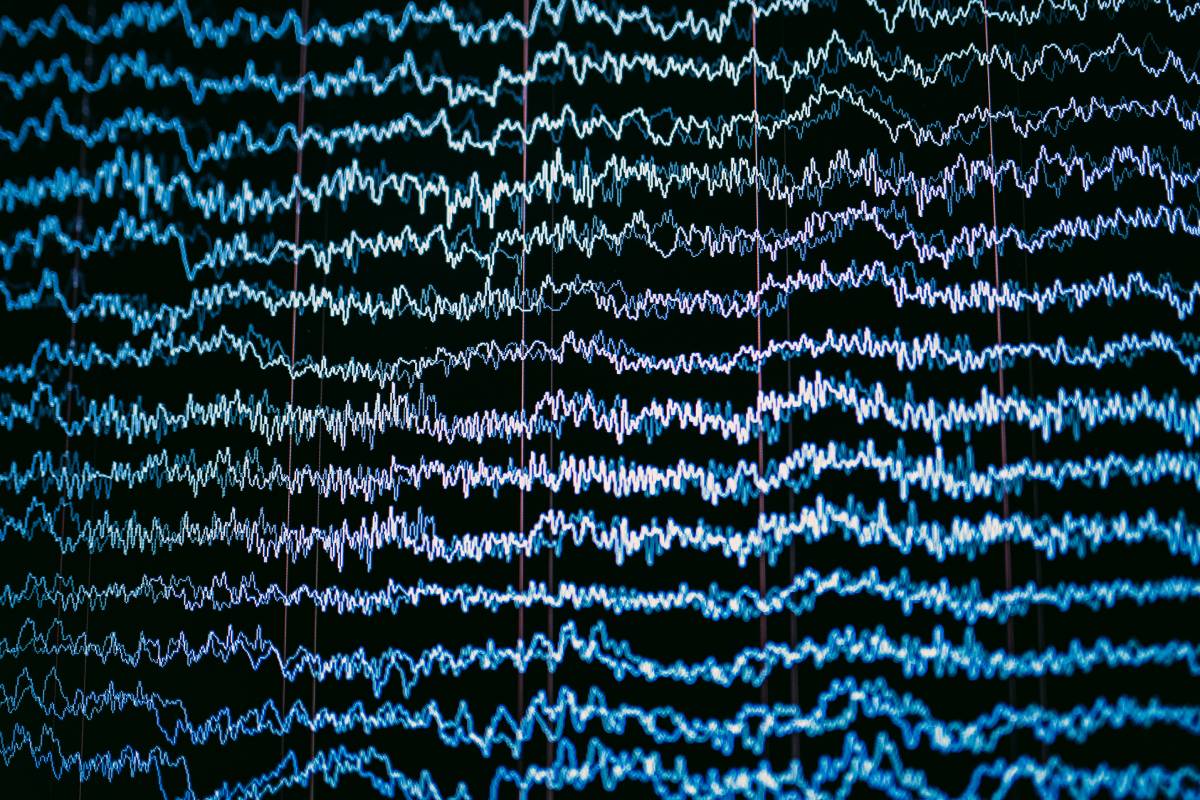
Electrophysiologic monitoring, or neuromonitoring, is employed during surgery to evaluate the functional integrity of the brain, brainstem, spinal cord, and peripheral and cranial nerves and to inform the anesthesiologist of the patient’s neurological state. To monitor brain activity, clinicians use electroencephalography (EEG). Several algorithms aim to compute a number that reflects level of consciousness from EEG data; however, clinicians may also directly interpret EEG for anesthesia monitoring.
Neuromonitoring has become common during many surgical procedures and has largely replaced intraoperative wake-up testing in spine surgery. This monitoring is carried out by a specialized team with specific expertise in the relevant techniques. In most cases, there is no established “standard of care” for intraoperative neuromonitoring. Techniques are selected by clinicians on a case-by-case basis to assess and protect at-risk structures.
EEG records electrical activity in the cerebral cortex and can detect ischemia and seizure activity, as well as reflect the effects of anesthesia on the brain for intraoperative monitoring purposes. Typically, electrodes are placed on the scalp in a standardized array before surgery. Each scalp electrode continuously records spontaneous brain activity from an area 2 to 3 cm in diameter.
Reductions in cerebral blood flow (CBF) cause rapid, characteristic changes in the EEG. With ischemia, there is a progressive decrease in synaptic activity, leading to the loss of high-frequency activity, a reduction in amplitude, and ultimately EEG silence. Depending on the severity of cerebral ischemia, specific changes in the EEG tracing are expected. The normal range for CBF is 35-70 mL/100g/min. When CBF is mildly decreased to 25-35 mL/100g/min, there may be a loss of beta frequencies on EEG, indicating mild, reversible neuronal injury. At a CBF of 18-25 mL/100g/min, EEG typically shows slowing in the theta range and decreased amplitudes, which corresponds to mild, reversible neuronal injury, with cell death expected within hours unless CBF is restored. When CBF drops to 12-18 mL/100g/min, further slowing to the delta range may be seen on EEG, along with decreased amplitudes, indicating moderate and reversible neuronal injury if addressed within a few hours. With a severe decrease in CBF to 8-12 mL/100g/min, EEG will show significant amplitude loss in all frequencies, corresponding to severe neuronal injury. Finally, when CBF falls below 8 mL/100g/min, there is a complete loss of activity on EEG, indicating significant and typically irreversible neuronal loss within minutes.
Anesthetic drugs influence EEG traces, enabling physicians to use EEG for monitoring the effects of anesthesia on the brain and thus indirectly estimate depth of anesthesia. Except for halothane, volatile agents initially increase the frequency of the frontal EEG. At higher doses,
this frequency decreases, and the amplitude diminishes. When approaching approximately 1.5 minimum alveolar concentration (MAC), burst suppression may appear on the EEG, and at even higher doses, electrical silence can be observed.
EEG monitoring is commonly employed during carotid endarterectomy to evaluate cerebral perfusion while the carotid artery is clamped. In this context, EEG slowing or asymmetry between the recordings on the operative side and the contralateral side can indicate ischemia. Additionally, EEG can be used during intracranial surgery to assess the cortex for signs of ischemia. However, a limitation of EEG monitoring is that surface recordings may not detect ischemia in subcortical regions.
References
Weinzierl MR, Reinacher P, Gilsbach JM, Rohde V. Combined motor and somatosensory evoked potentials for intraoperative monitoring: intra- and postoperative data in a series of 69 operations. Neurosurg Rev. 2007 Apr;30(2):109-16; discussion 116. doi: 10.1007/s10143-006-0061-5. Epub 2007 Jan 13. PMID: 17221265.
Lall RR, Lall RR, Hauptman JS, Munoz C, Cybulski GR, Koski T, Ganju A, Fessler RG, Smith ZA. Intraoperative neurophysiological monitoring in spine surgery: indications, efficacy, and role of the preoperative checklist. Neurosurg Focus. 2012 Nov;33(5):E10. doi: 10.3171/2012.9.FOCUS12235. PMID: 23116090.
Jameson LC, Sloan TB. Monitoring of the brain and spinal cord. Anesthesiol Clin. 2006 Dec;24(4):777-91. doi: 10.1016/j.atc.2006.08.002. PMID: 17342964.
Barkley GL, Baumgartner C. MEG and EEG in epilepsy. J Clin Neurophysiol. 2003 May-Jun;20(3):163-78. doi: 10.1097/00004691-200305000-00002. PMID: 12881663.
Bootin ML. Deep brain stimulation: overview and update. J Clin Monit Comput. 2006 Oct;20(5):341-6. doi: 10.1007/s10877-006-9031-2. Epub 2006 Sep 2. PMID: 16951905.
Harper CM. Intraoperative cranial nerve monitoring. Muscle Nerve. 2004 Mar;29(3):339-51. doi: 10.1002/mus.10506. PMID: 14981732.